About Target-to-B!

Target-to-B!
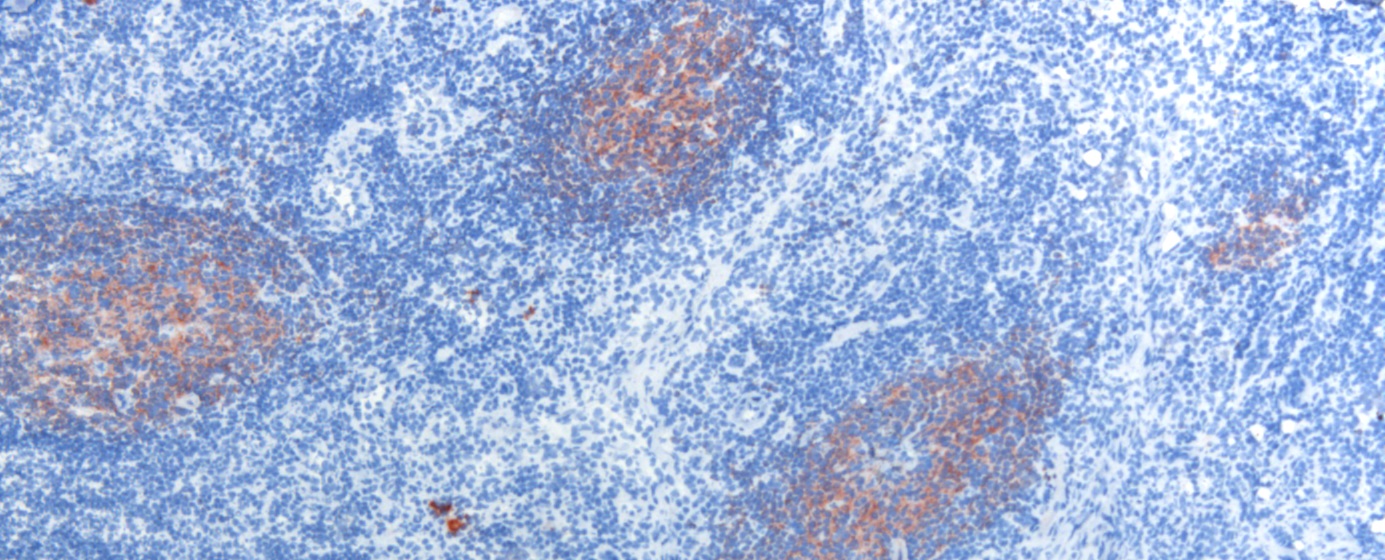
B cells exert multiple essential functions in our immune system: production of protective antibodies, immunomodulatory cytokines, and antigen-presentation to T cells. Dysregulated activation of B cells forms the basis of a wide variety of B-immune-mediated diseases (B-IMD) characterized by production of disease-causing pathogenic autoantibodies or oncogenic transformation of B cells in various malignancies (B-ONC). The crucial role of B-cells and antibodies in B-IMD/B-ONC pathology is evident from the clinical observation that B-cell and IgG-targeted therapies can be highly effective. Therefore, B cell dysfunction is the central theme of our ‘out-of-balance’ research program, whereby we take the parallels in pathogenesis and treatment strategies across different B-IMDs as well as between B-IMDs and B-ONCs as a critical starting point.
At present, the underlying pathogenic mechanisms in B-IMDs and B-ONCs, their commonalities and differences in cellular functionality, remain unknown. Moreover, functional consequences of structural characteristics of antibodies, e.g. the extent and role of antibody glycosylation, in immune activation are undefined. A coherent pathophysiological underpinning of why, where, and when B cell or antibody-targeting strategies are effective is missing.
Incorporating COVID-19 into our research
The current pandemic with COVID has turned society on its head worldwide. There is a lot of uncertainty and a lot of uncertainty. In particular, patients and their practitioners have tried to get good advice and treatments without much specific prior knowledge of this new coronavirus: SARS-CoV2. As Jaap van Dissel of the RIVM so beautifully described: we are driving by looking in the rearview mirror. Understanding what has happened should help to carve the future to properly counter COVID. In the meantime, we considered it very prudent to obtain more insight into the maintenance of SARS-CoV-2-specific immunity after primo-infection for the patient cohorts of our T2B program. Several questions remain to be answered. What does immunosuppression on the SARS-CoV2 immunity? How big is the risk of reinfection by the virus under the use of immunosuppression?
It is unknown how long the adaptive virus-specific immunity will last and thus protect against re-infection. That’s true in general, but this uncertainty is more pregnant for the large group of immune-suppressed patients. In addition, the long-awaited national vaccination program against SARS-CoV-2 to pursue group immunity is likely to be less effective in patients, based on experience with previous vaccinations.
For this reason we submitted a ZonMW application partly from T2B, which was honored in July. Health Holland has also granted matching, which makes it possible for our patients to obtain more clarity about COVID in the next two years. The purpose of this ZonMW COVID study is to answer the question of whether the course of SARS-CoV-2-specific immunity differs over time in immune-suppressed patients compared to healthy individuals and whether the efficacy of SARS-CoV-2-targeted vaccination in these patients in the coming year will be similar to that in healthy individuals. We will compare these responses with the course of humoral and cellular immunity in healthy people, with which the results are relevant to the whole of society. To this end we use the unique platform of the T2B consortium, a close collaboration and infrastructure of 6 different academic hospitals, RIVM and Sanquin Blood Supply Foundation. In a prospective observational large study, we will collect longitudinal clinical data and blood samples that will be used to monitor vaccination responses in smaller subgroups in detail, both in patients and healthy controls, with and without previous SARS-CoV-2 infection. With this additional study from T2B, our goal is to provide guidance and advice regarding practical limitations (social distancing), medication effects, and vaccination strategies (one, multiple), not only for our patients, but for the entire community.
This project has received funding from the PPP allowance (Health Holland), the Association of Dutch Health Foundations (SGF) and our private partners Pfizer B.V., Janssen Vaccines & Prevention B.V., Acerta Pharma B.V, Fresenius and Fluidigm
Our consortium
Our B cell consortium includes both clinical, translational and fundamental research groups and companies, together with various patient organisations. We are thus combining our strength in immunology, hemato-oncology, diagnostics and clinical experience. Patients from various B-IMD/B-ONC cohorts of ongoing studies will be studied over a longer period of time for clinical (outcome measures) and state-of-the-art immunological, biochemical and molecular parameters. Clinical data and materials collected longitudinally in the past and from current inclusions will be available for our network.
Our joint expertise in both relatively common (e.g. rheumatoid arthritis, pemphigus-like disorders, chronic lymphatic leukemia) and rare (e.g. idiopathic thrombocytopenic purpura, autoimmune-encephalitis, multiple sclerosis, autoimmune nephritis, follicular lymphoma) diseases enables a better definition of common principles and pathways operative to improve disease-specific and/or patient-tailored treatment outcomes.
Our ambition is (i) to integrate and expand current knowledge on these diseases, (ii) to establish a harmonized immune monitoring platform and (iii) to provide mechanistic understanding to predict outcome and develop innovative treatment modalities.
This should lead to major advances of our insight into B-IMD/B-ONC pathogenesis and to significant improvement of therapy efficacy for these serious diseases.
The T2B program aims to provide disease-overarching underpinnings and to create a solid basis for targeted and effective treatment protocols. For example, novel ‘biologicals’ or small-molecule inhibitors targeting BCR-signaling (inhibitors of BTK, PI3K) or B-cell survival show clinically proven efficacy in B-ONCs (1-3). It is currently not clear in which B-IMDs or at which disease-stage these compounds could also be therapeutically applied. By introduction of B-cell oncology expertise into the B-IMD field , novel therapeutic targets in B-IMD could be uncovered. Conversely, development of improved therapeutic options for B-ONC patients will benefit from harmonized immunomonitoring, and increased fundamental insight into B-cell biology.
Early therapy tailoring for non-responder patients would greatly enhance therapy efficacy. Moreover, alternative B-cell-targeting strategies are needed in B-IMD/B-ONC to secure the best outcome with least side-effects.
